UVEITIS AND RED EYES
- Zeenat Shah
- Jan 22
- 2 min read
Early Diagnosis of Uveitis
Uveitis refers to inflammation of the uveal tract of the eye, which includes the iris, ciliary body, and choroid. Early diagnosis is crucial to prevent complications such as vision loss, glaucoma, cataracts, or retinal damage. Here's an overview of its early diagnosis and treatment:
Signs and Symptoms of Uveitis
Early signs of uveitis can vary depending on the specific type, but common symptoms include:
Anterior uveitis (iritis):
Redness in the eye.
Pain and sensitivity to light (photophobia).
Blurred vision.
Excess tearing.
Intermediate uveitis:
Floaters in vision.
Blurred vision.
Minimal pain or redness (often absent).
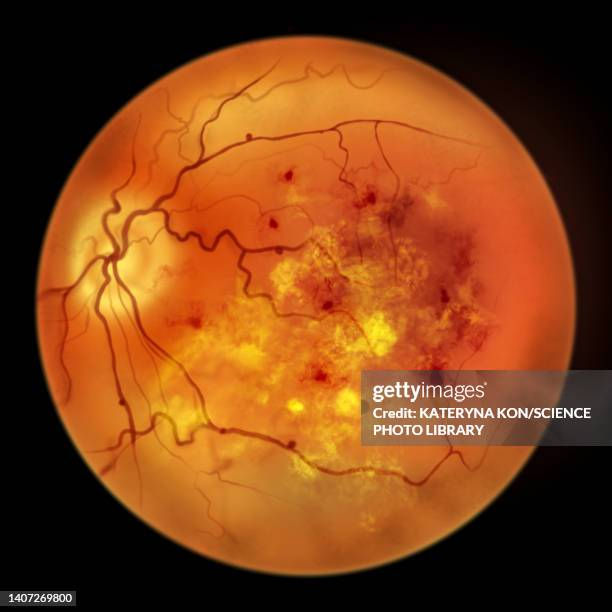
Posterior uveitis:
Floaters and reduced vision.
Dark spots in the visual field.
Inflammation in the retina or choroid.
Panuveitis:
Involves all parts of the uvea, combining symptoms from anterior, intermediate, and posterior types.
Diagnostic Steps
Early detection requires:
Patient History:
Symptoms onset and duration.
Associated systemic conditions (e.g., autoimmune diseases, infections).
Recent infections or trauma.
Family history of autoimmune disorders.
Clinical Examination:
Slit-lamp biomicroscopy: To identify inflammation in the anterior segment.
Dilated fundus examination: To examine the posterior segment for retinal or choroidal involvement.
Tonometry: To measure intraocular pressure (important in detecting secondary glaucoma).
Laboratory Tests:
Blood tests: Look for infectious or autoimmune markers (e.g., HLA-B27 for ankylosing spondylitis).
Imaging: Optical coherence tomography (OCT) or fluorescein angiography for posterior uveitis.
Systemic Evaluation:
Collaboration with rheumatologists or infectious disease specialists for systemic causes (e.g., sarcoidosis, tuberculosis, syphilis).
Treatment of Uveitis
Treatment focuses on reducing inflammation, managing the underlying cause, and preventing complications.
1. Initial Management
Topical corticosteroids (e.g., prednisolone eye drops) for anterior uveitis.
Cycloplegic agents (e.g., atropine or cyclopentolate) to relieve pain and prevent synechiae.
2. Systemic Therapy
Oral corticosteroids for more severe cases or posterior involvement.
Immunosuppressive drugs (e.g., methotrexate, cyclosporine) for chronic or autoimmune-related uveitis.
3. Targeted Biological Therapy
Anti-TNF agents (e.g., adalimumab) for refractory uveitis, particularly in autoimmune cases.
4. Antimicrobial Treatment
For infectious causes (e.g., antibiotics for bacterial infections, antivirals for herpes, or antitubercular therapy).
5. Surgical Intervention
Vitrectomy may be necessary in cases of severe posterior uveitis or complications such as retinal detachment.
Importance of Early Intervention
Prevents Vision Loss: Early diagnosis and treatment reduce the risk of permanent damage to ocular structures.
Improves Prognosis: Early management of systemic associations (e.g., rheumatoid arthritis, Behçet’s disease) can significantly improve overall health outcomes.
Reduces Recurrence: Adequate control of the first episode lowers the likelihood of relapses.


Author- Titanium eye care


Comments